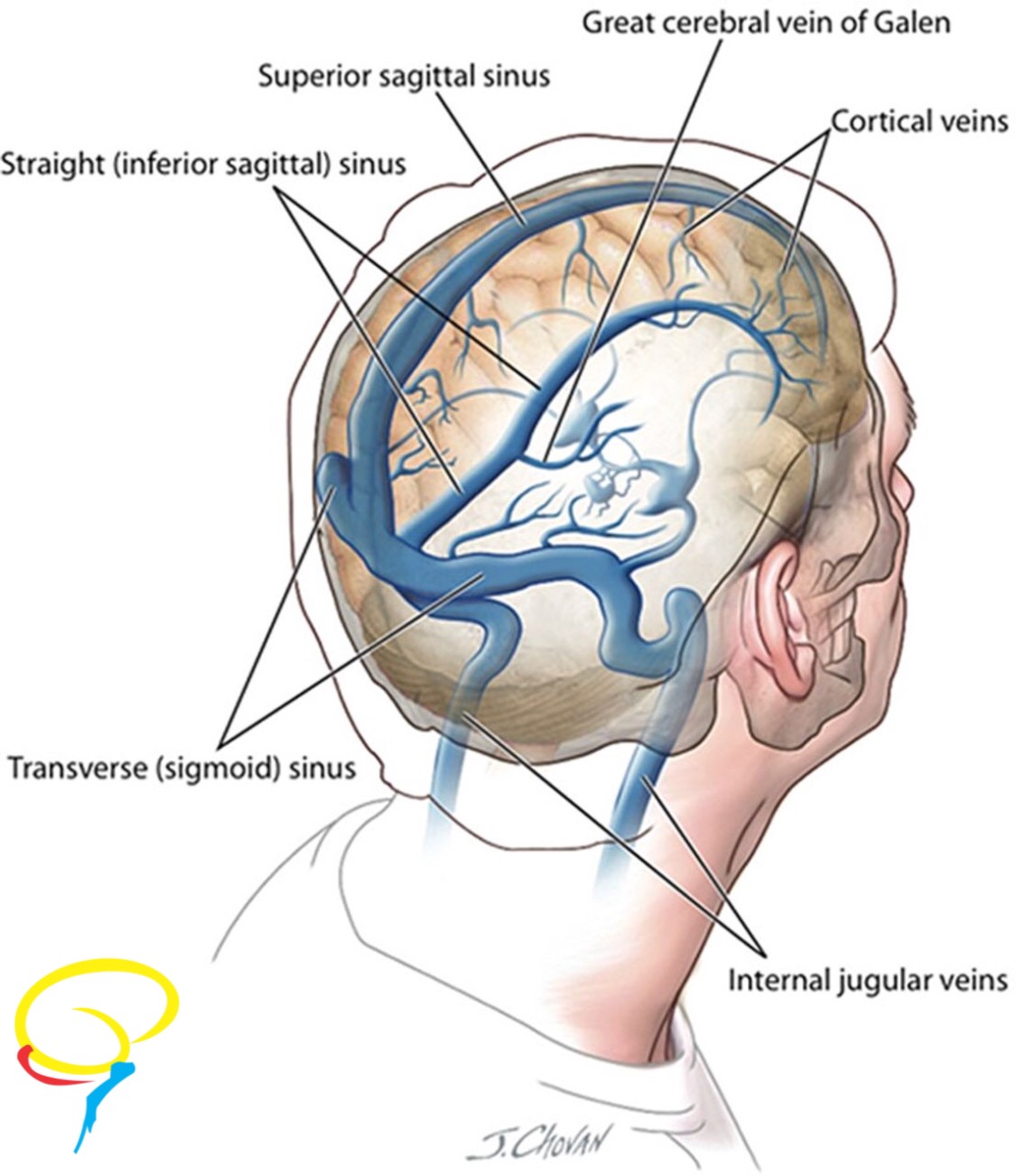
In regular conditions, blood is pumped from the heart and carried to the brain by the arteries blood, supplying oxygen and nutrients. Once this function is completed, blood is collected by small cerebral veins, that drain it into larger veins called dural sinuses (Figure 1).
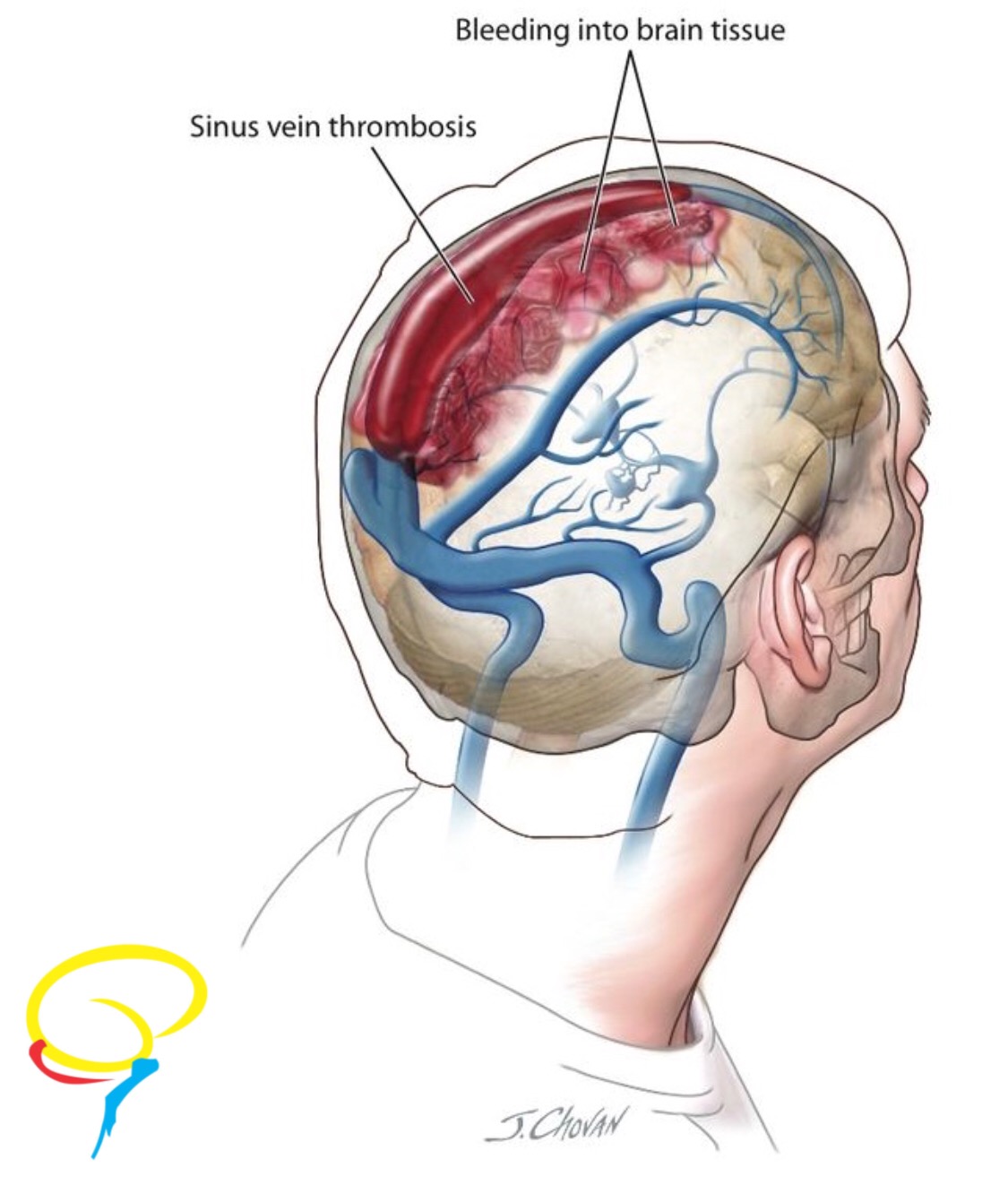
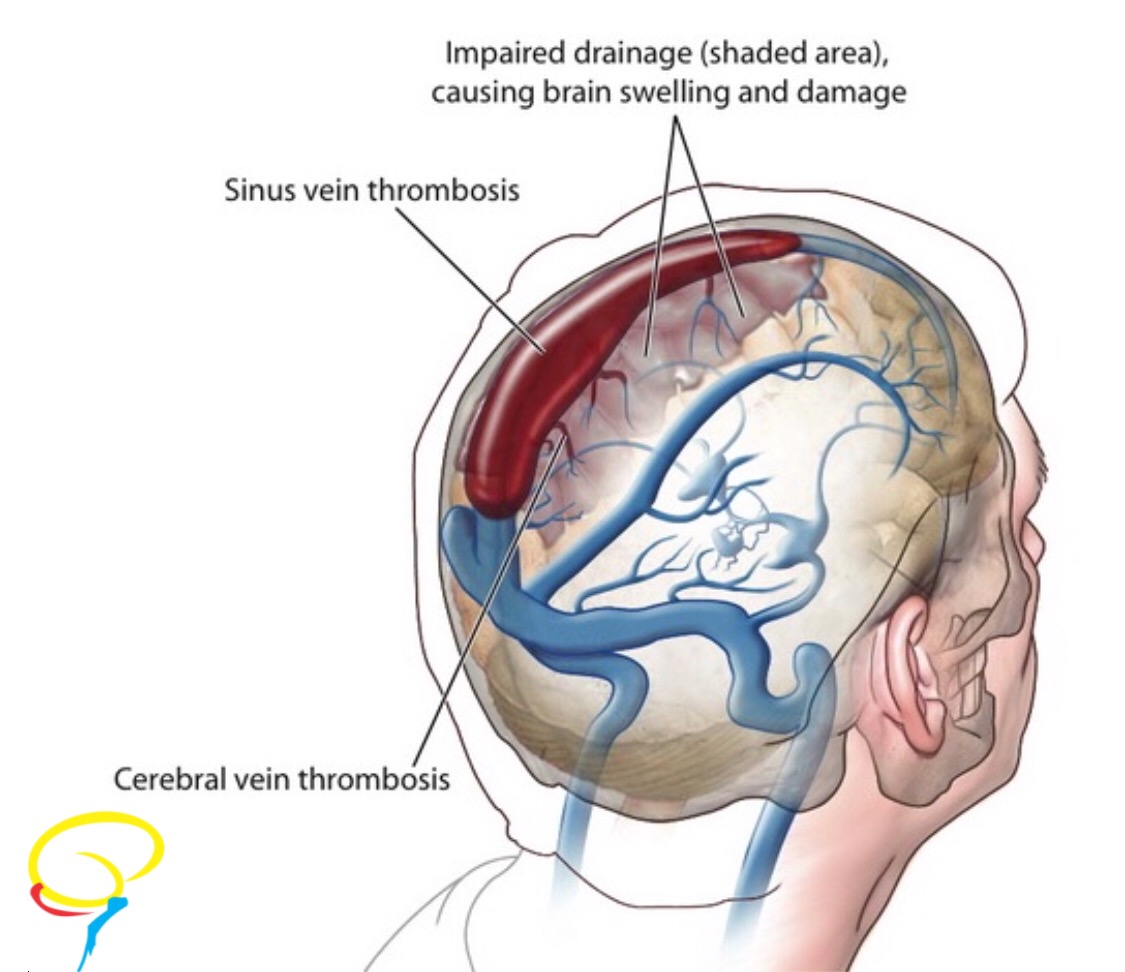
The blockage of the blood flow by a clot in the head veins, leads to an increase in blood pressure in vessels in the area just before the blockage. This increase in pressure blood leads to the swelling of parts of the brain, causing headaches; high blood pressure can damage the brain tissue, leading to symptoms similar to those of a stroke (figure 2) and finally, to the rupture and bleeding of the blood vessel (Figure 3).
The most common symptom is an intense headache, but also nausea, vomiting, blurred vision and neurological deficits may occur (i.e. similar to the symptoms of a stroke). In very severe cases, it can lead to coma or even death.
The causes are divided into risk factors: (1) temporary and (2) permanent (genetic). In newborns, the clot is most commonly caused by an infection. In adults, risk factors include abnormal blood coagulation (such as thrombophilias), use of birth control pills, use of estrogen-containing therapies or patches, pregnancy and puerperium, active cancer and certain medications (such as tamoxifen and chemotherapy).
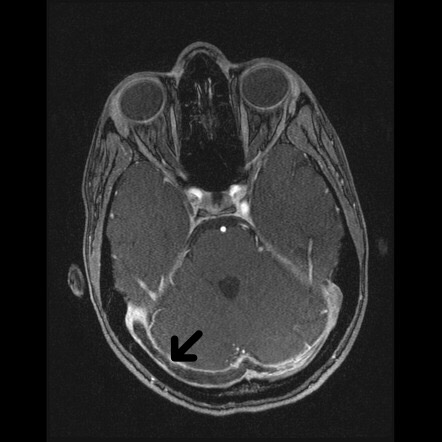
Diagnosis may be made based on imaging tests, such as magnetic resonance angiography (MRA) (Figure 4), Computed Tomography (CT), or cerebral angiography, through which the clot can be seen within the affected vein, due to the injection of contrast material.
Immediate treatment consists of the administration of “blood thinners” (known as anticoagulants). In the first days, intravenous heparin or injections under the skin (subcutaneously) are used. The purpose of administering anticoagulants is to prevent the clot from growing and new clots from being formed. The clot will be slowly dissolved by the body over the weeks and months.
Drugs that stimulate the dissolution of the clot (known as fibrinolytic drugs) are usually not administered because they may increase the risk of bleeding in the brain.
Radiological or surgical procedures with catheters to remove the clot (called mechanical thrombectomy) are performed only in severe cases and in patients who present a worsening condition even under adequate blood fluidization therapy.
Once the patient is stable for a few days, an oral blood anticoagulant is administered.
In this point, the main issue is the length of the treatment with this medication. If the clot was caused by a temporary risk factor (such as an infection or use of birth control pills), using it for 3 to 6 months is sufficient.
If the risk factor is genetic, long-term therapy with thrombophilia is preferred.
Almost 80% of patients are fully recovered, but it may take several weeks or months to return to normal conditions. Headaches and seizures may persist for some time and become chronic.